Kidneys pathology. (Subject 17) презентация
Содержание
- 2. Lecture Plan
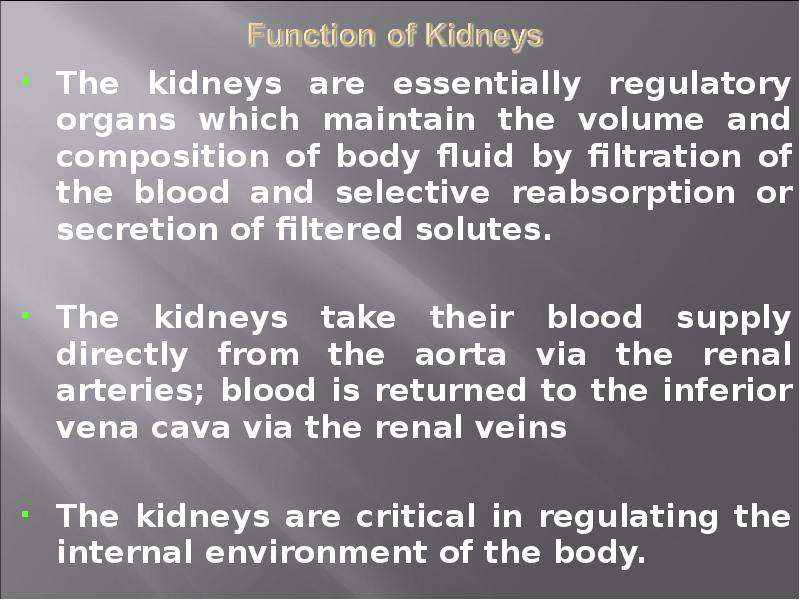
- 3. The kidneys are essentially regulatory organs which maintain the volume and
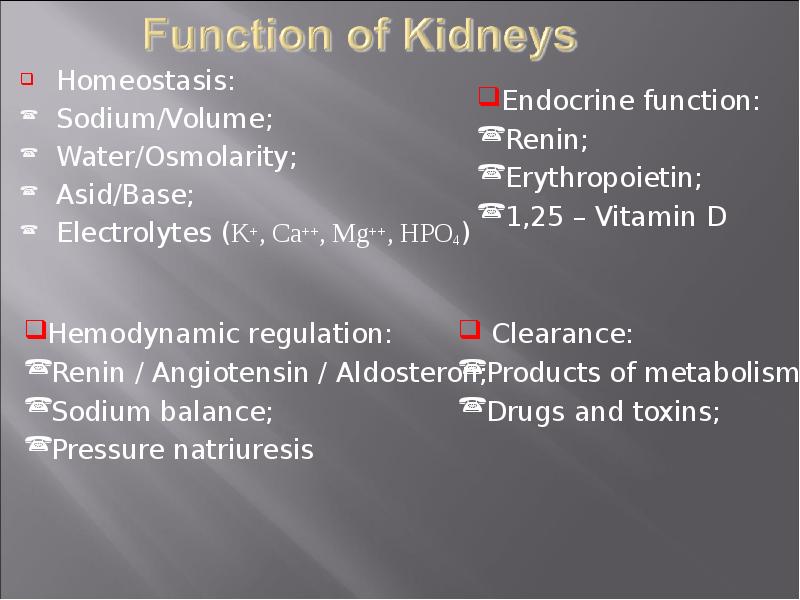
- 4. Homeostasis: Homeostasis: Sodium/Volume; Water/Osmolarity; Asid/Base; Electrolytes (K+, Ca++, Mg++, HPO4)
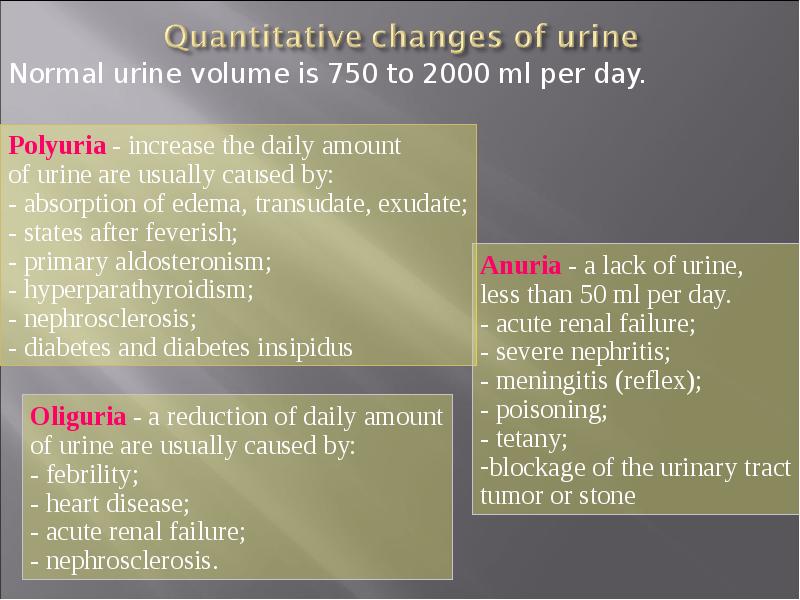
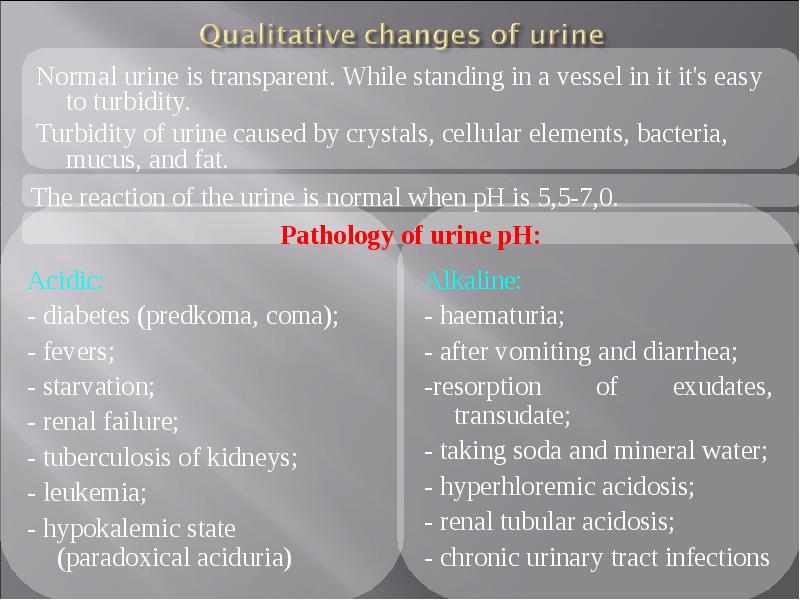
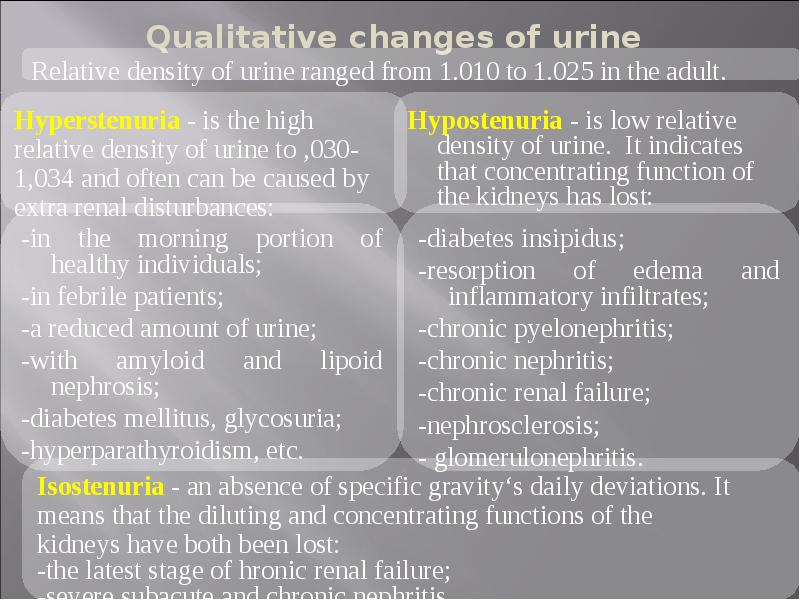
- 5. Normal urine volume is 750 to 2000 ml per day.
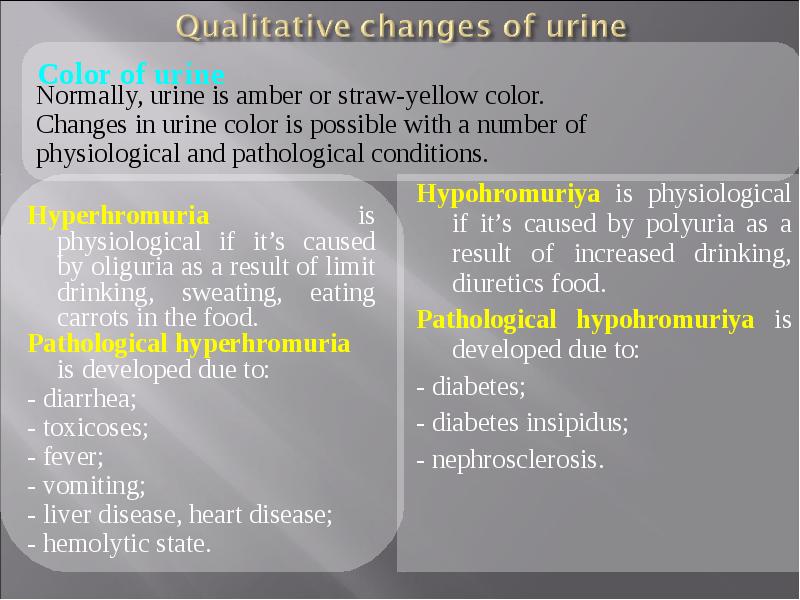
- 6. Hypohromuriya is physiological if it’s caused by polyuria as a result
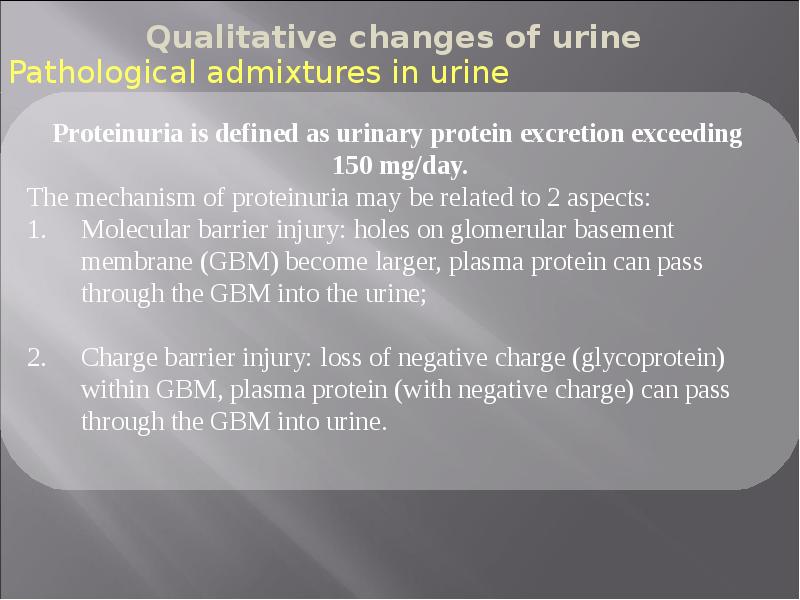
- 10. Nonpathological proteinuria - excessive protein excretion is apparently not the result
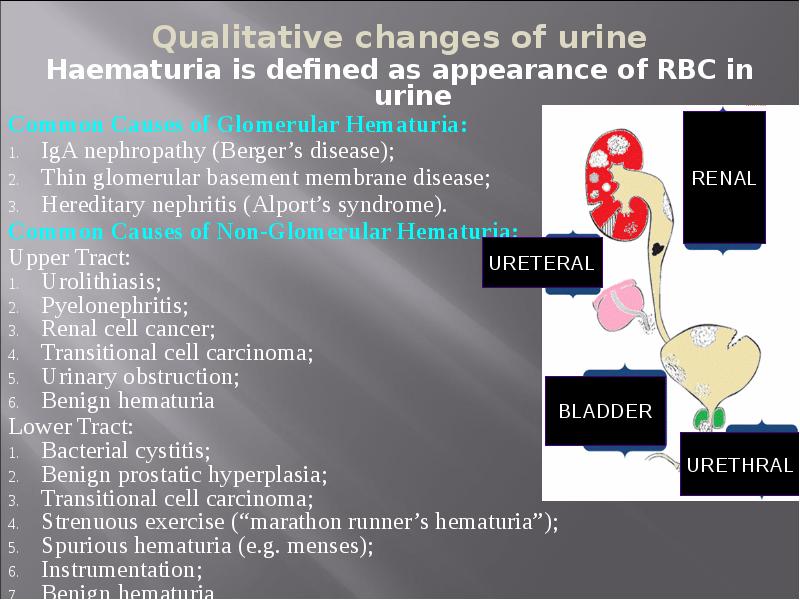
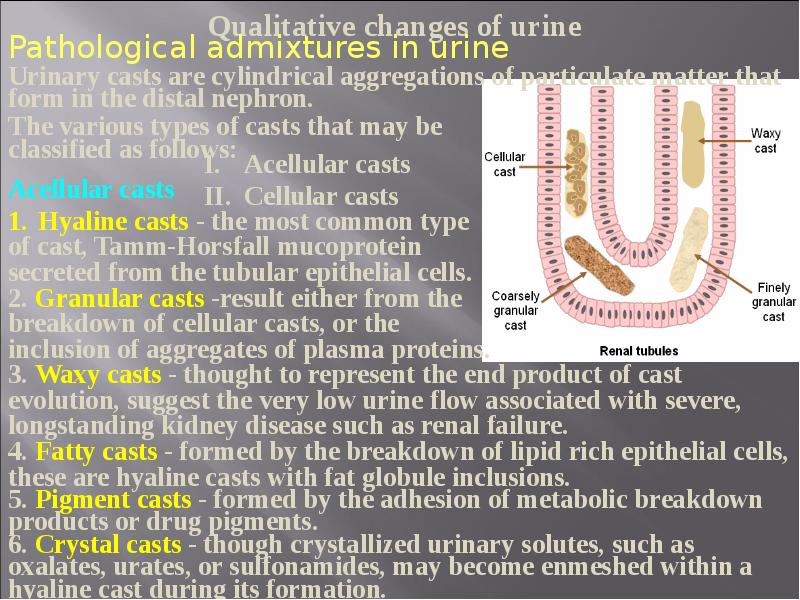
- 11. Haematuria is defined as appearance of RBC in urine Haematuria
- 12. Visible (macroscopic) haematuria (VH) Visible (macroscopic) haematuria (VH) Non-visible (microscopic) haematuria
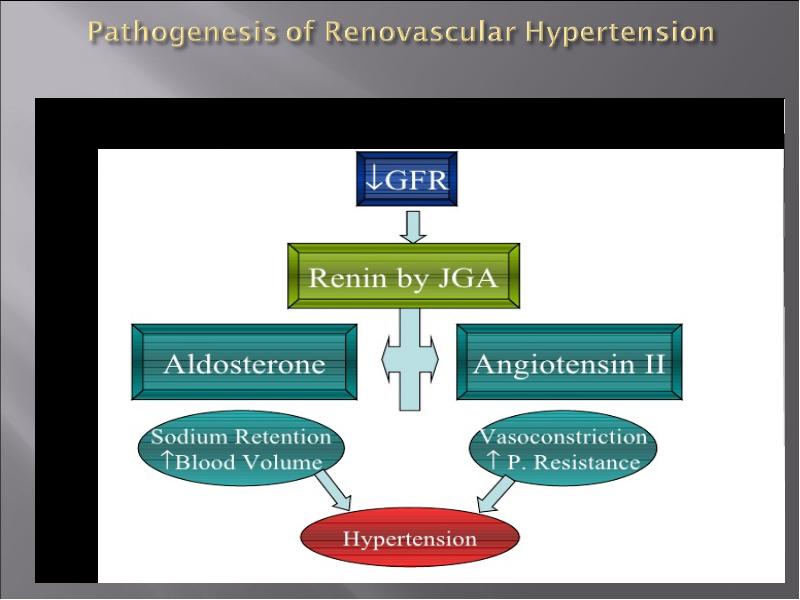
- 17. Clinical: Clinical: 1. Primary - are caused by kidney pathology (acute
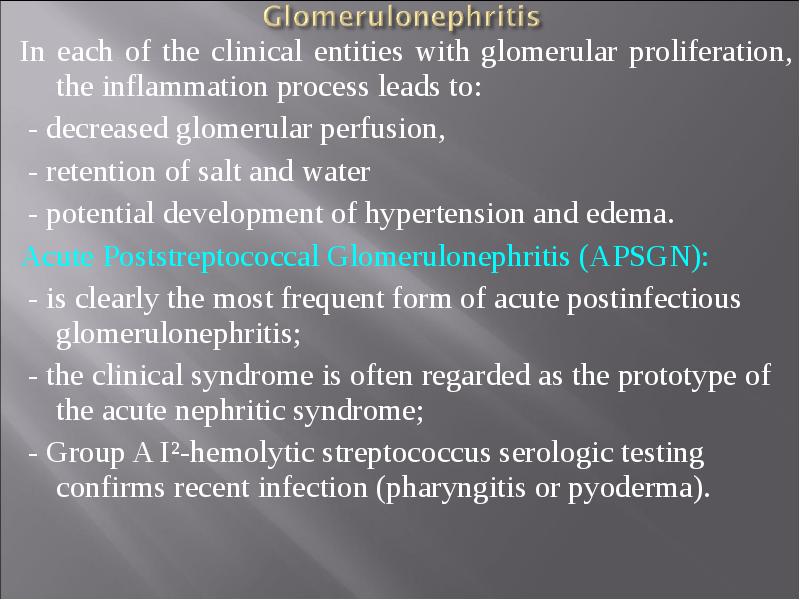
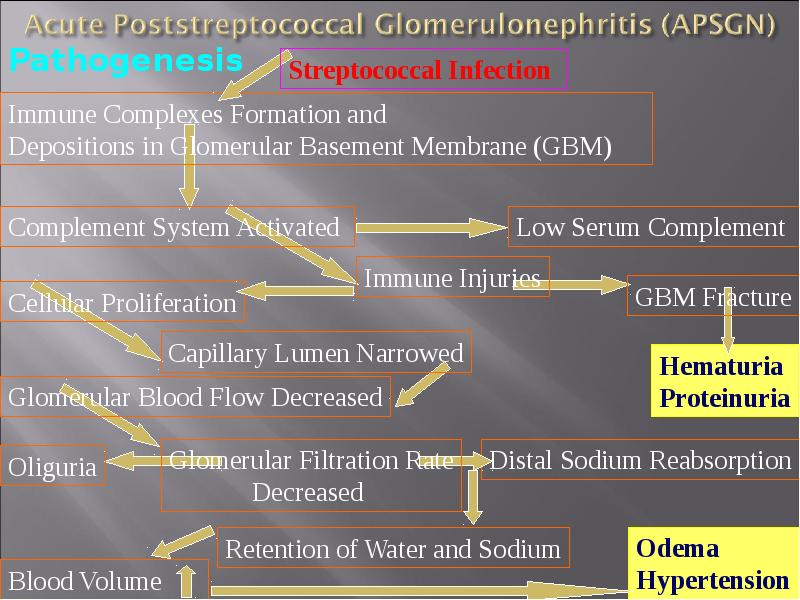
- 18. In each of the clinical entities with glomerular proliferation, the inflammation
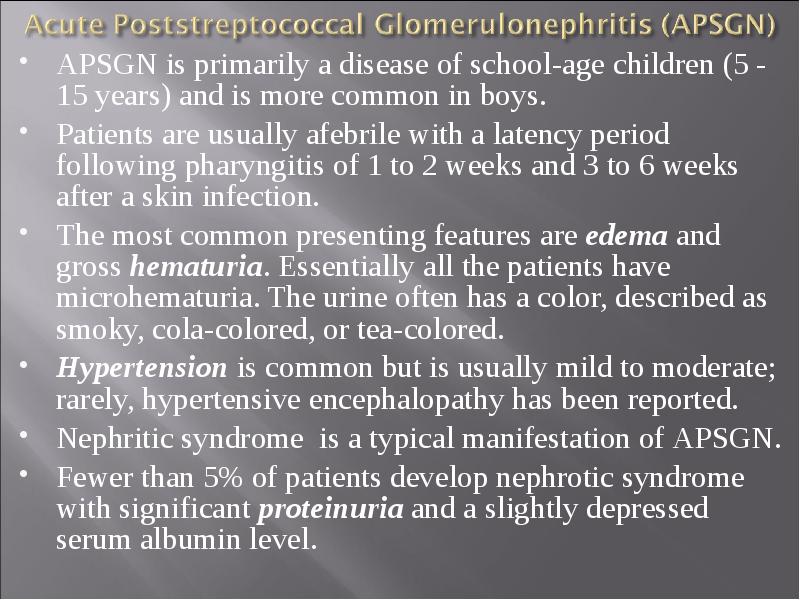
- 19. APSGN is primarily a disease of school-age children (5 - 15
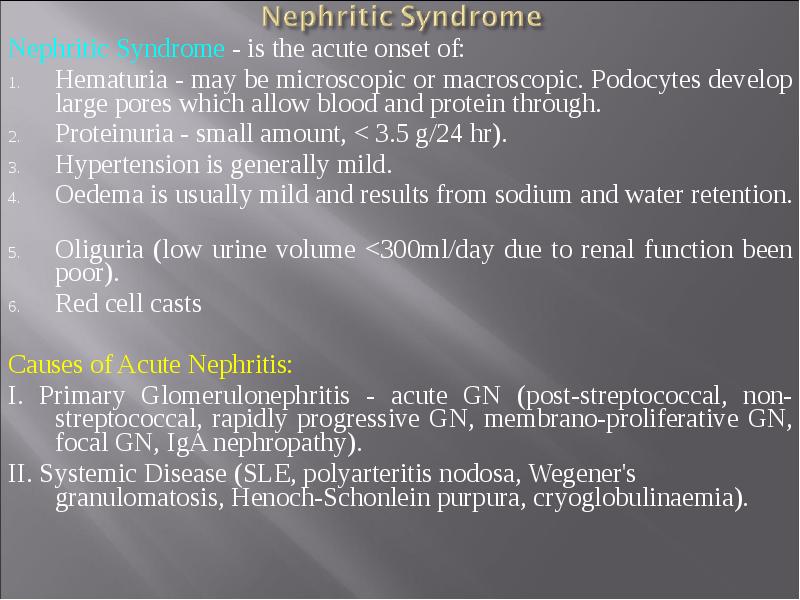
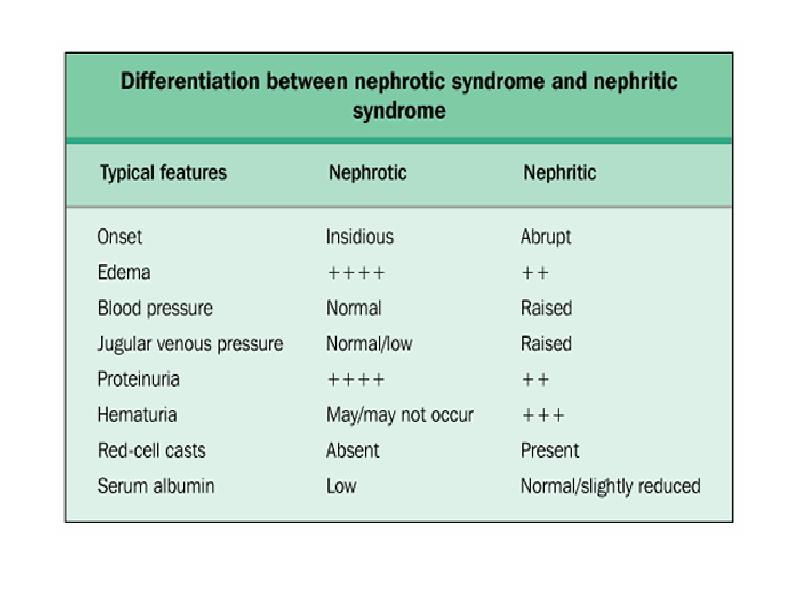
- 21. Nephritic Syndrome - is the acute onset of: Nephritic Syndrome -
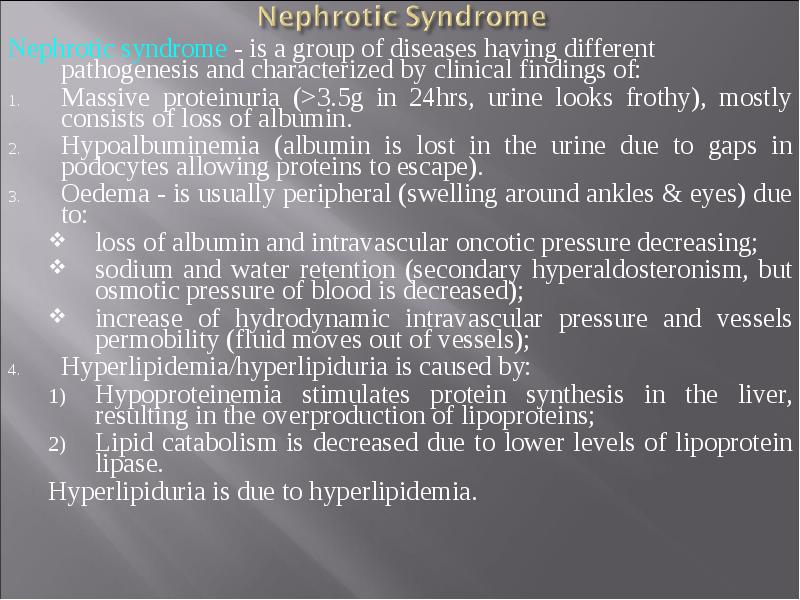
- 22. Nephrotic syndrome - is a group of diseases having different pathogenesis
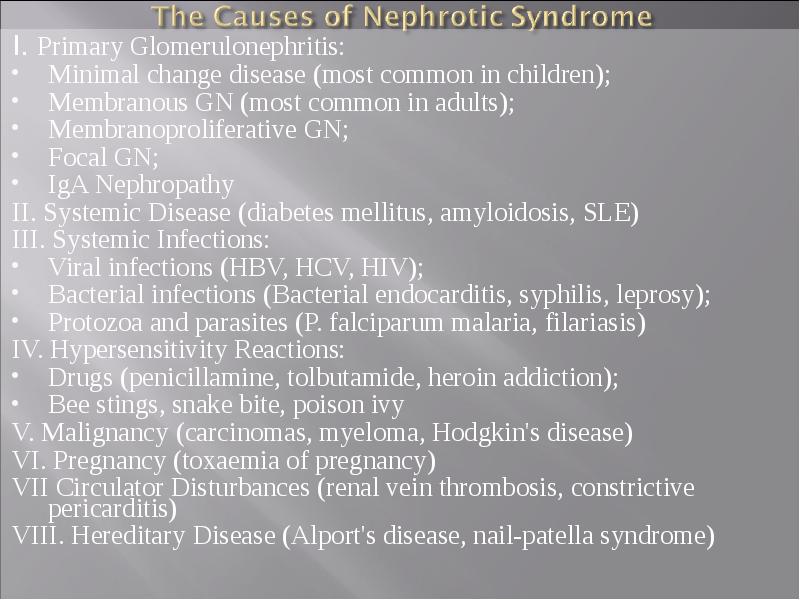
- 23. I. Primary Glomerulonephritis: I. Primary Glomerulonephritis: Minimal change disease (most common
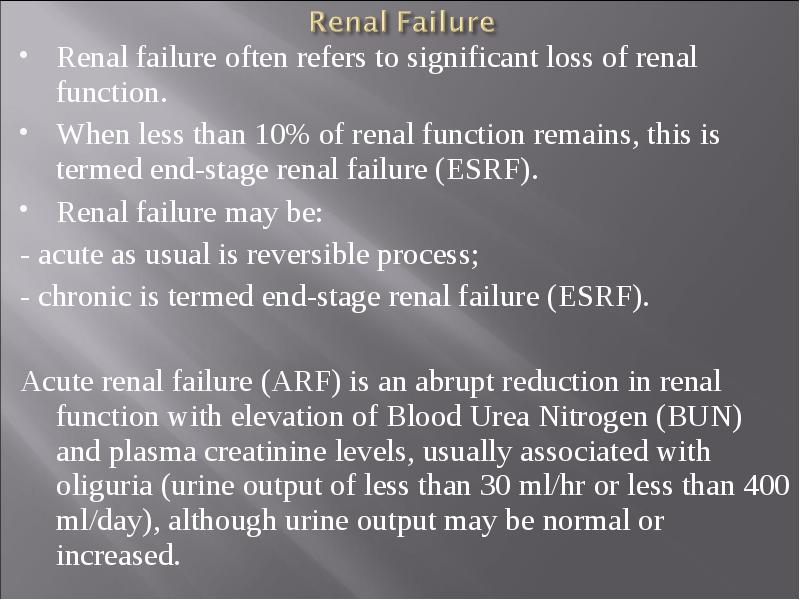
- 25. Renal failure often refers to significant loss of renal function.
- 26. Acute renal failure commonly is classified as: Acute renal failure commonly
- 28. Pathophysiology and Clinical manifestations of Uremic syndrome Pathophysiology and Clinical manifestations
- 29. Retention of nitrogenous wastes Retention of nitrogenous wastes Increased intracellular Na+
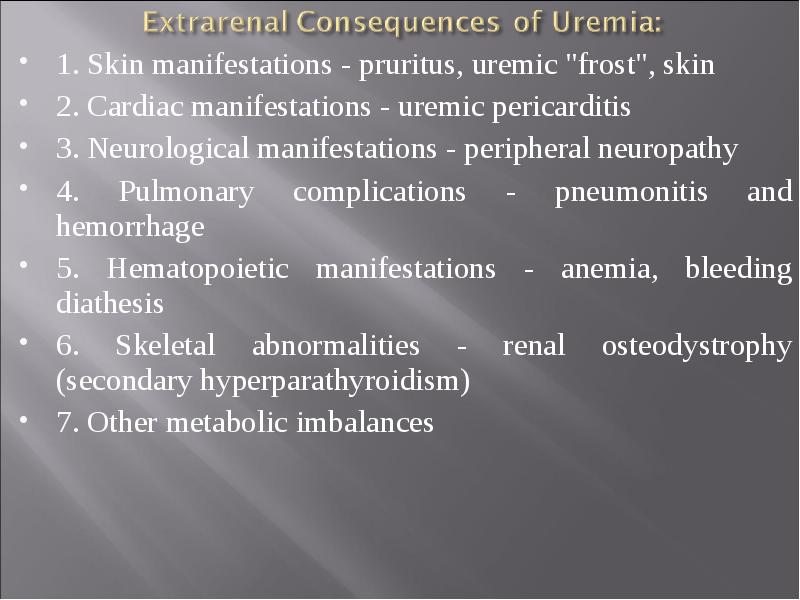
- 30. 1. Skin manifestations - pruritus, uremic "frost", skin 1. Skin
- 32. Thank you for your attention Thank you for your attention
- 33. Скачать презентацию
Слайды и текст этой презентации
Похожие презентации