Atopic dermatitic презентация
Содержание
- 2. Definition Atopic dermatitis is a chronic, pruritic inflammatory skin disease
- 3. Epidemiology affects up to 25% of children and 2–3% of adults
- 4. Pathogenesis complex genetic, immunologic, and environmental factors dysfunctional skin barrier
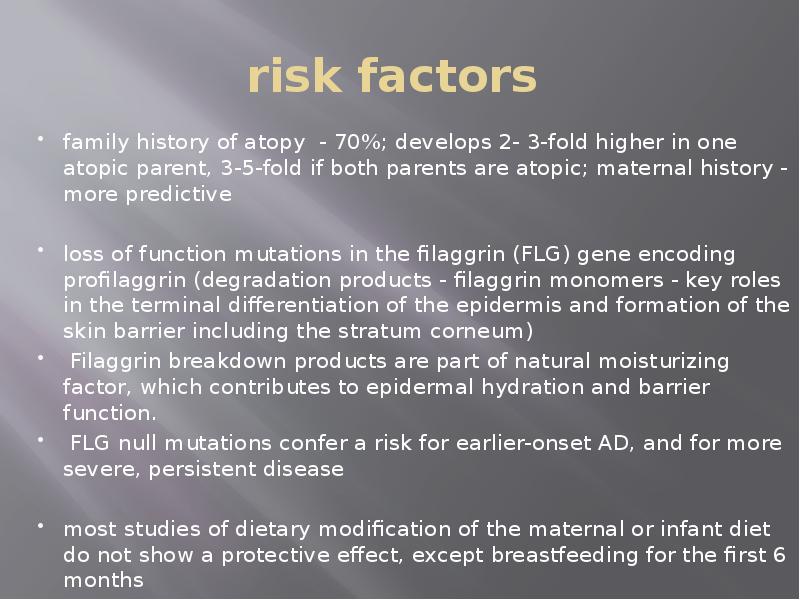
- 5. risk factors family history of atopy - 70%; develops 2-
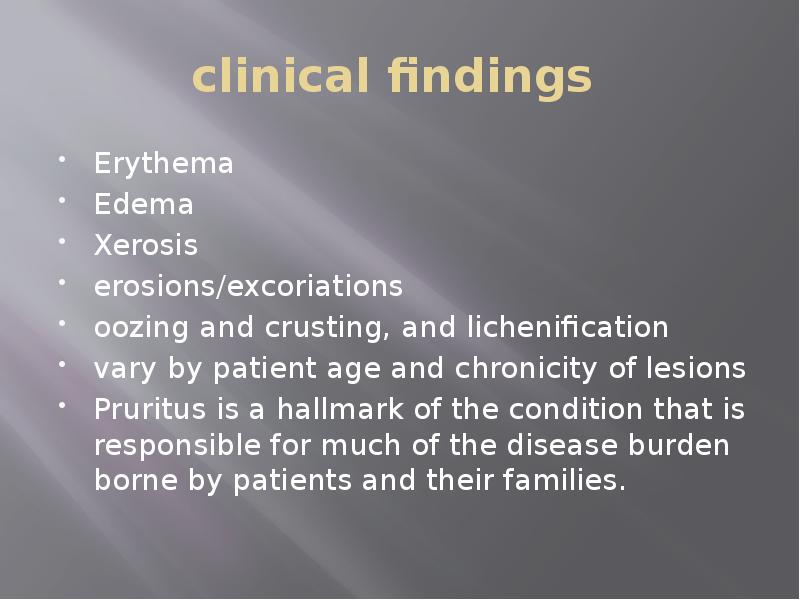
- 6. clinical findings Erythema Edema Xerosis erosions/excoriations oozing
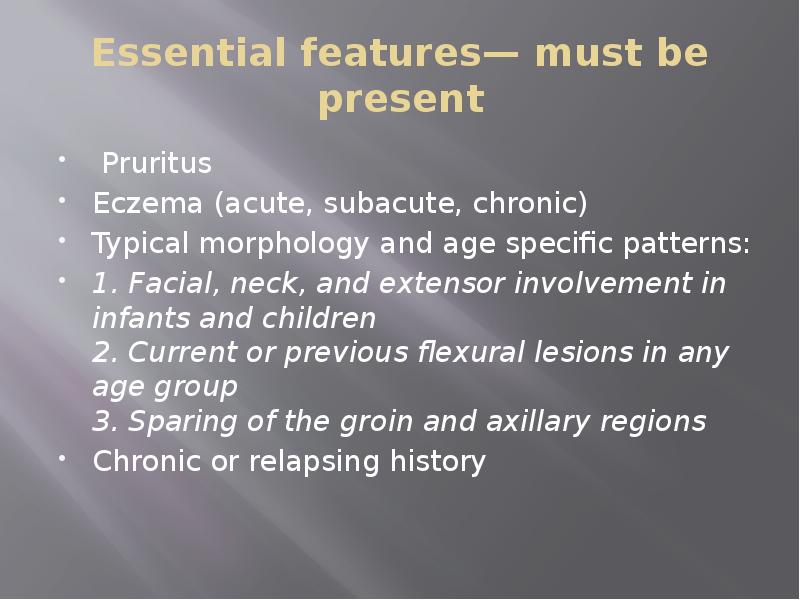
- 7. Essential features— must be present Pruritus Eczema (acute, subacute, chronic) Typical
- 10. Important features seen in most cases, adding support to the diagnosis:
- 11. Associated features help to suggest the diagnosis of atopic dermatitis but
- 12. Exclusionary conditions • Scabies • Seborrheic dermatitis • Contact dermatitis (irritant
- 13. Patients with presumed atopic dermatitis should have their diagnosis based on
- 14. Common associations/comorbidities food allergies, asthma, and allergic rhinitis/rhinoconjunctivitis. AD can be
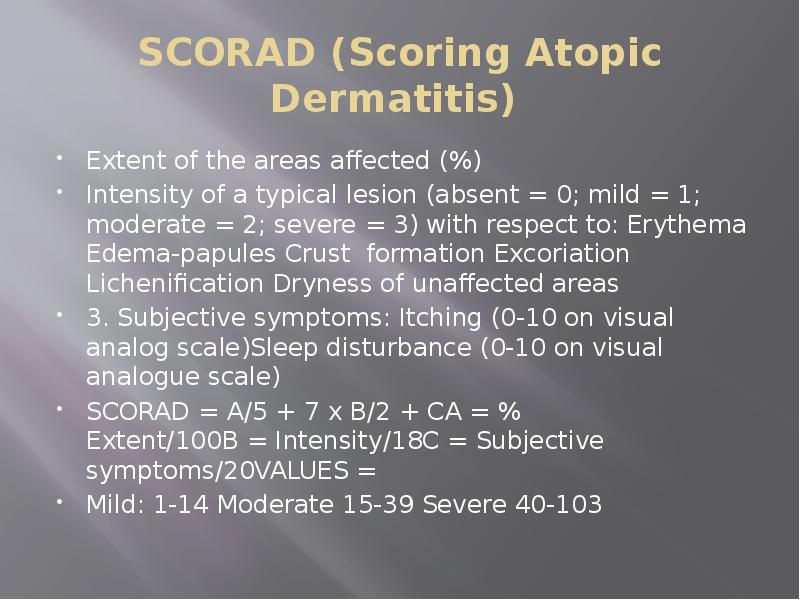
- 15. SCORAD (Scoring Atopic Dermatitis) Extent of the areas affected (%) Intensity
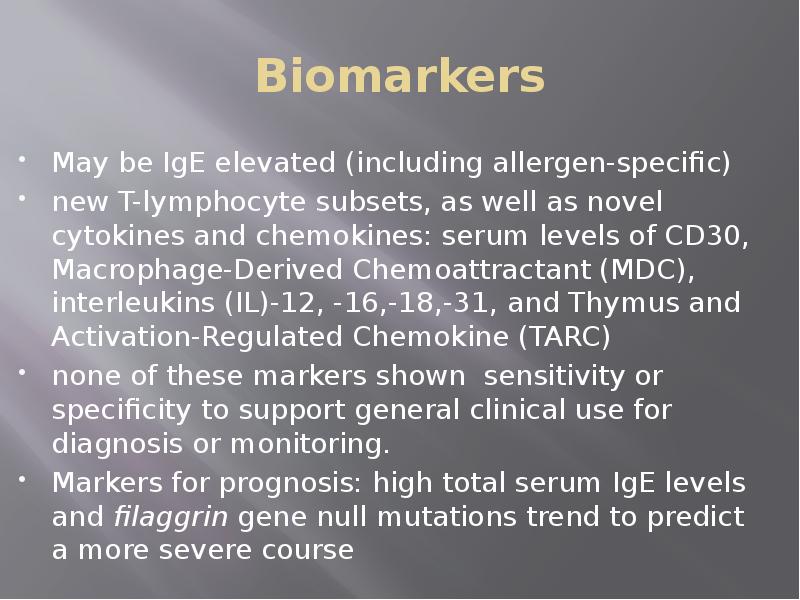
- 16. Biomarkers May be IgE elevated (including allergen-specific) new T-lymphocyte subsets, as
- 17. Topical corticosteroids for patients who failed to respond to good skin
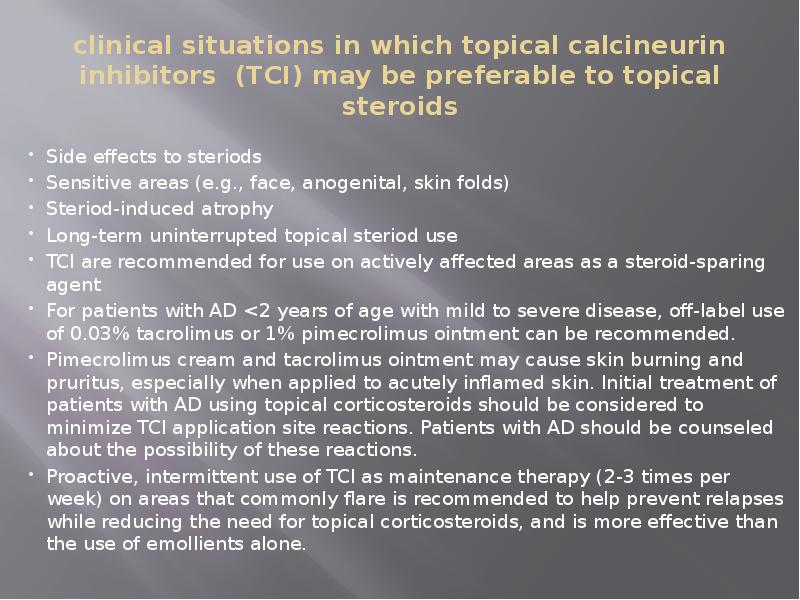
- 18. clinical situations in which topical calcineurin inhibitors (TCI) may be preferable
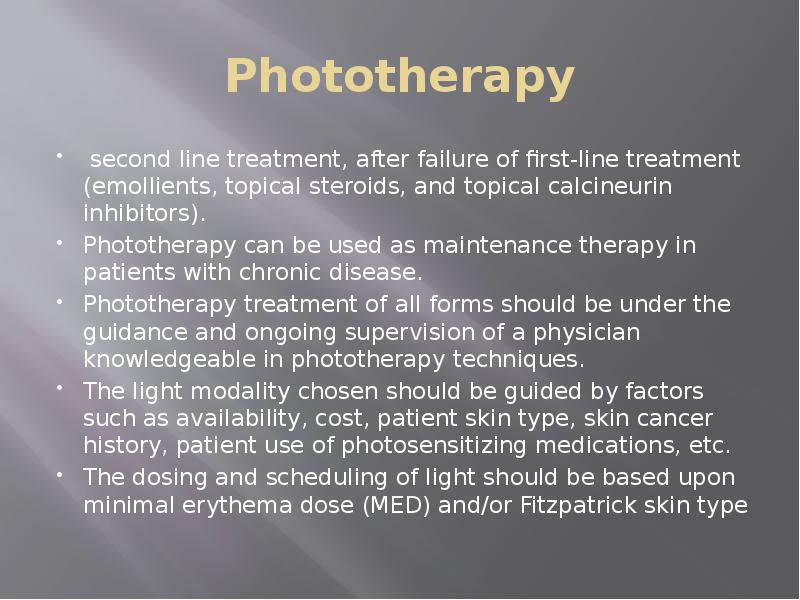
- 19. Phototherapy second line treatment, after failure of first-line treatment (emollients, topical
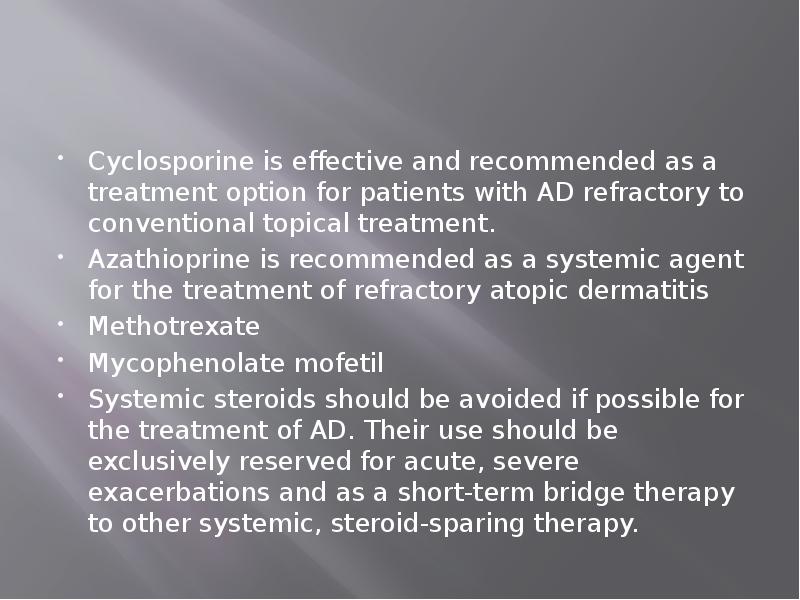
- 20. Cyclosporine is effective and recommended as a treatment option for patients
- 23. Скачать презентацию



Слайды и текст этой презентации
Похожие презентации