Infectious exanthema in children презентация
Содержание
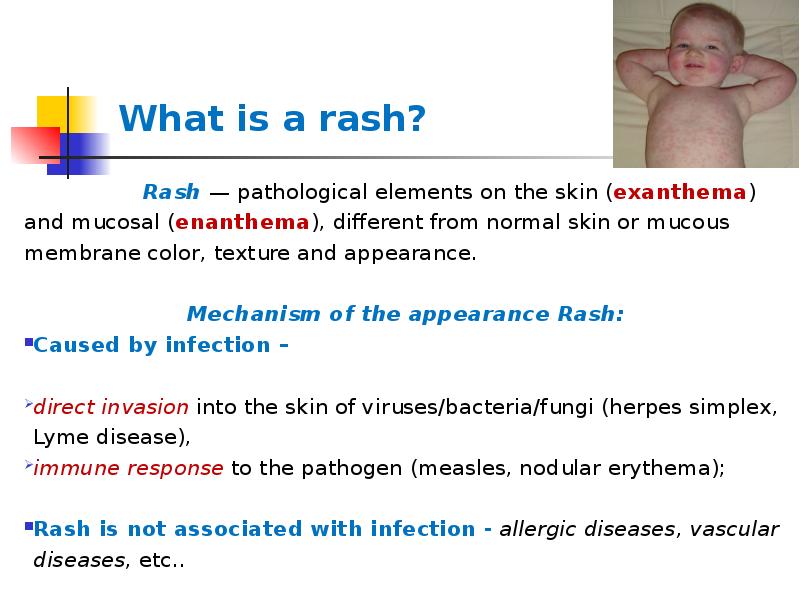
- 2. What is a rash? Rash — pathological
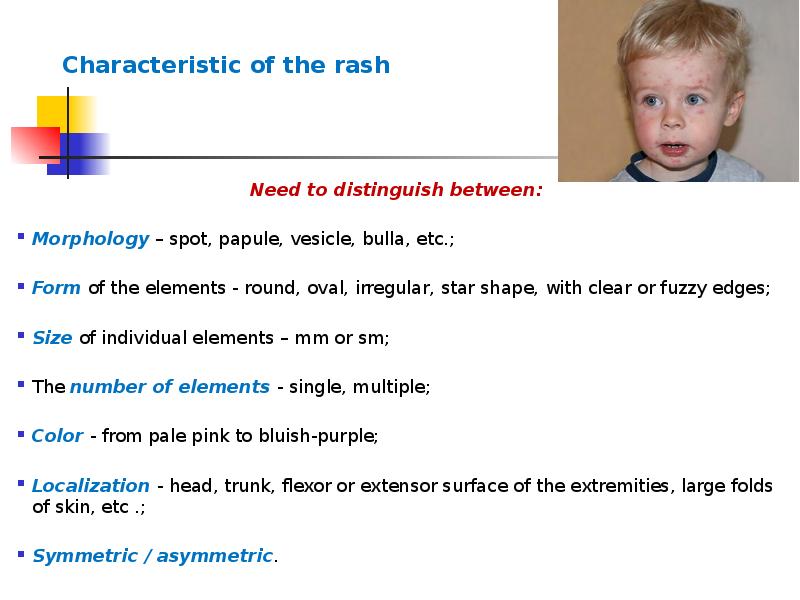
- 3. Characteristic of the rash Need to distinguish between: Morphology –
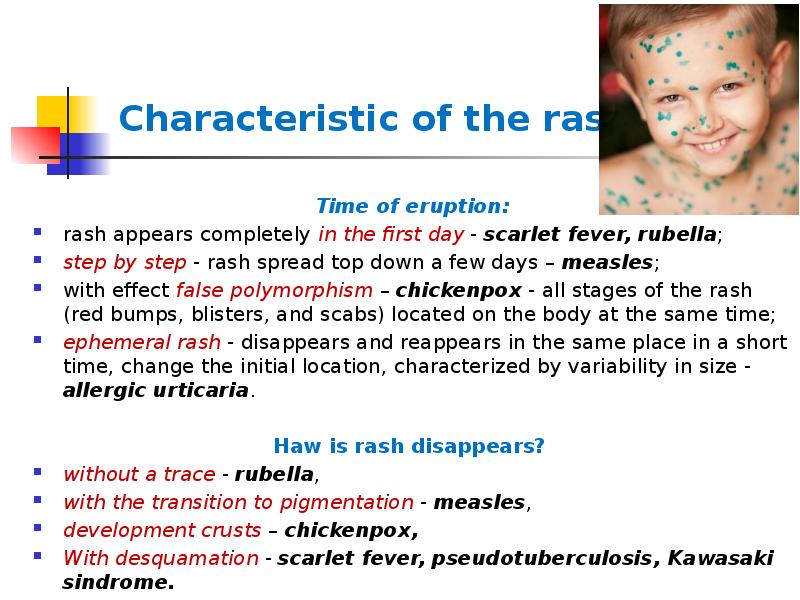
- 4. Characteristic of the rash Time of eruption: rash appears completely
- 5. Scarlet fever МКБ-10 (А38)
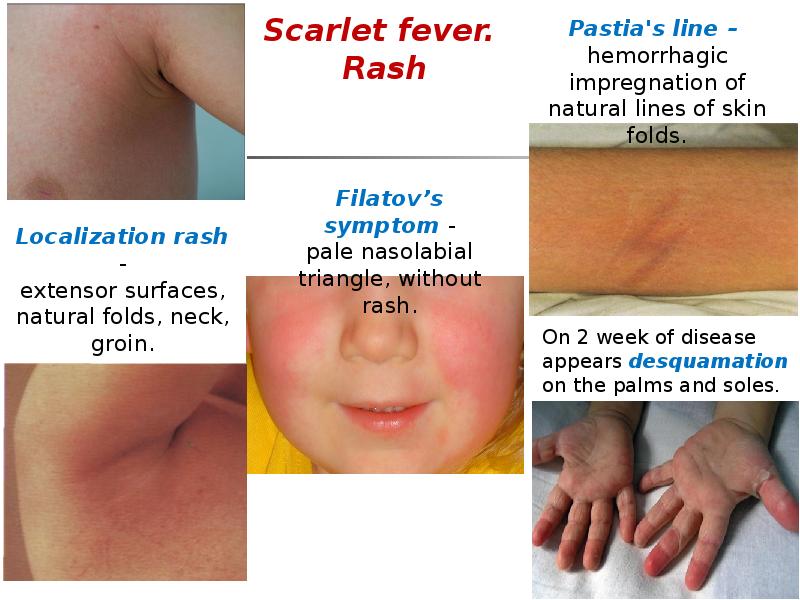
- 6. Scarlet fever. Rash
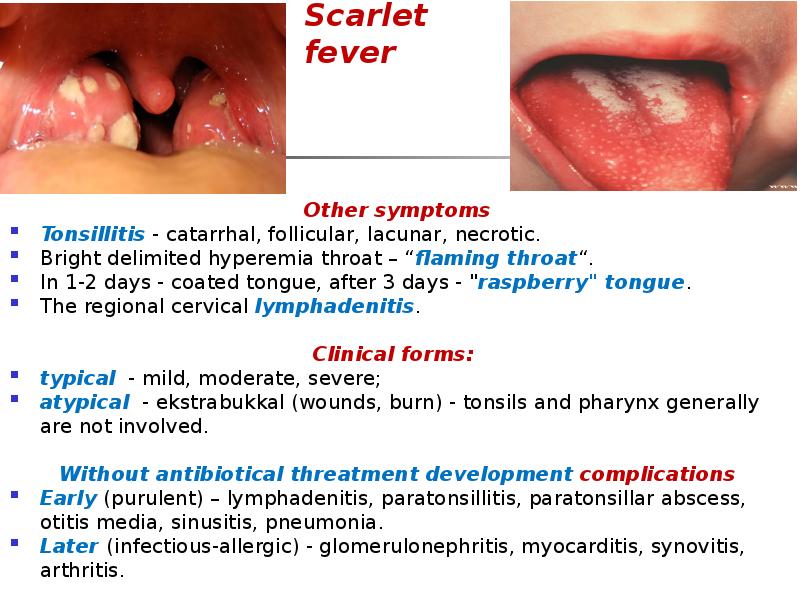
- 7. Scarlet fever Other symptoms Tonsillitis - catarrhal, follicular, lacunar, necrotic. Bright
- 8. Scarlet fever Diagnosis CBC – leukocytosis, shift to the left,
- 9. PSEUDOTUBERCULOSIS МКБ-10 (A04.8, A28.2) Pseudotuberculosis - is characterized by polymorphism
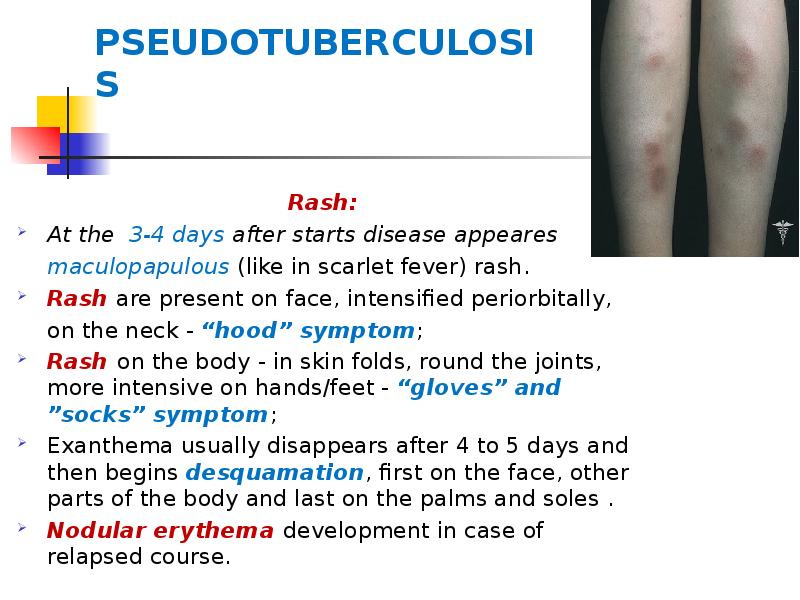
- 10. PSEUDOTUBERCULOSIS Rash: At the 3-4 days after starts disease appeares maculopapulous
- 11. Other simptoms Catarrhal syndrome - pharyngeal and tonsil erythema (without
- 12. PSEUDOTUBERCULOSIS
- 13. PSEUDOTUBERCULOSIS Laboratory data CBC: leucocytosis, neutrophilia with left shift, eosynophilia, ERS
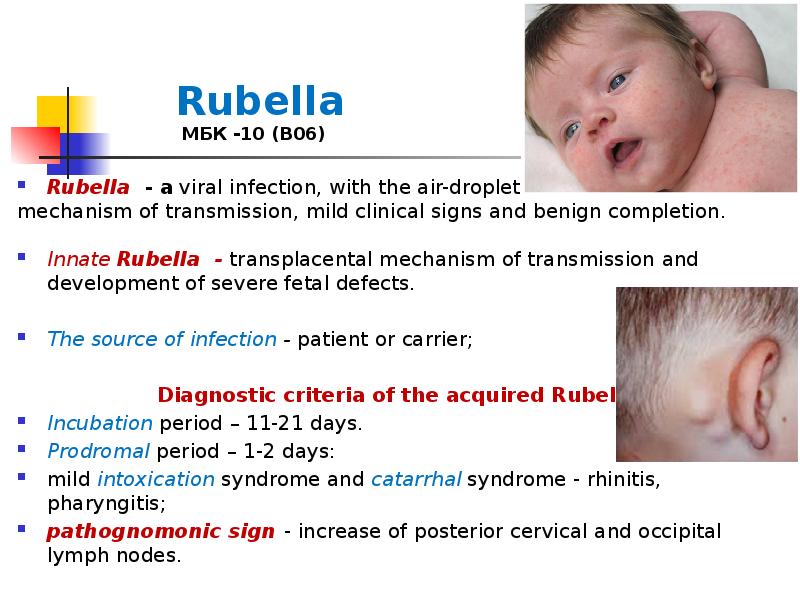
- 14. Rubella МБК -10 (В06) Rubella - a viral infection, with the
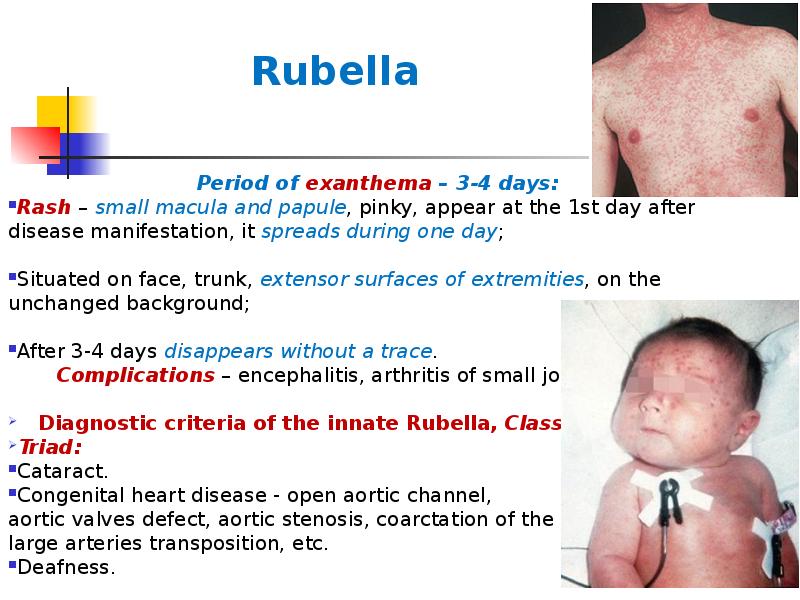
- 15. Rubella Period of exanthema – 3-4 days: Rash – small macula
- 16. Rubella Confirmation of the diagnosis: 1. CBC - leucopenia, lymphocytosis, plasmatic cells,
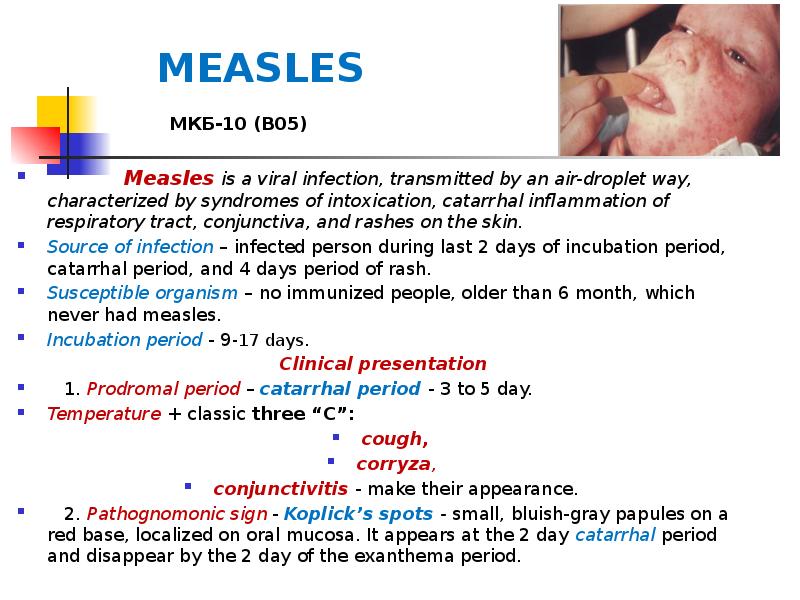
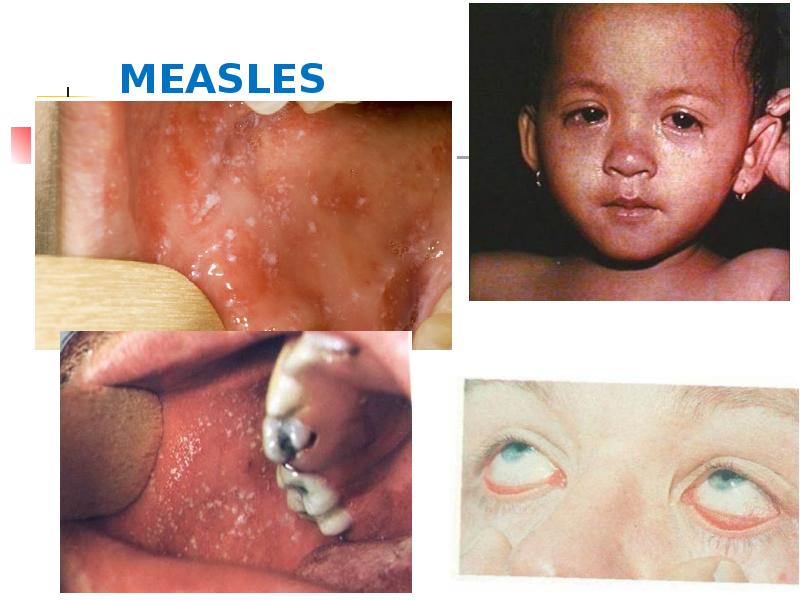
- 17. MEASLES МКБ-10 (В05) Measles is a viral
- 18. MEASLES
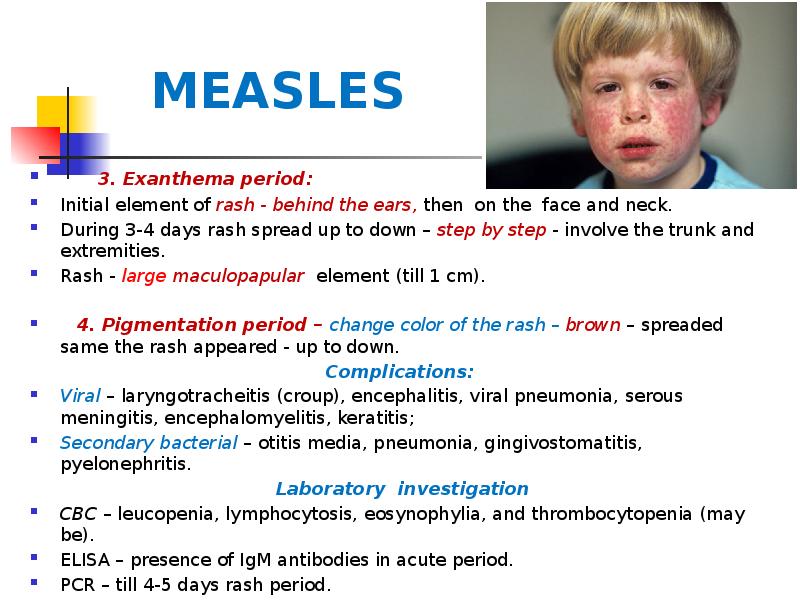
- 19. MEASLES 3. Exanthema period: Initial element of rash -
- 20. MEASLES
- 21. MEASLES Treatment Noncomplicated mild, moderate measles and atypical forms do not
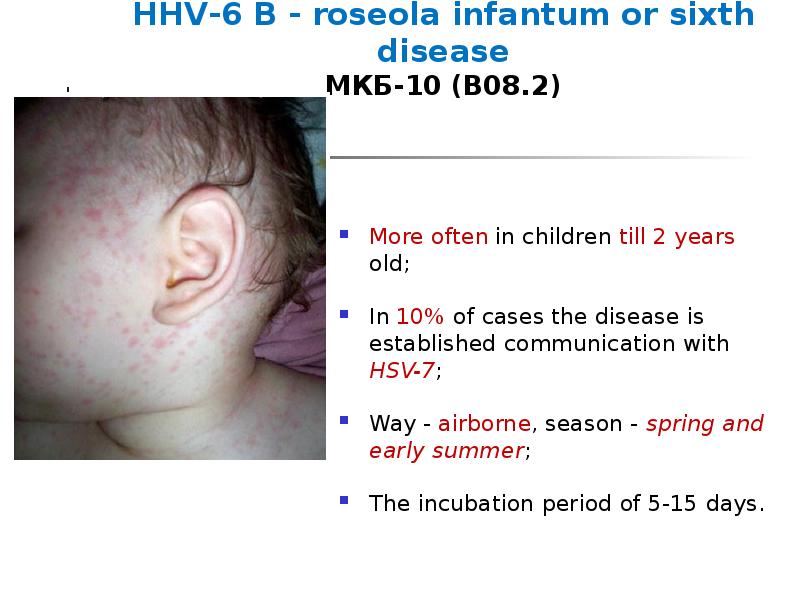
- 22. HHV-6 В - roseola infantum or sixth disease МКБ-10 (В08.2) More
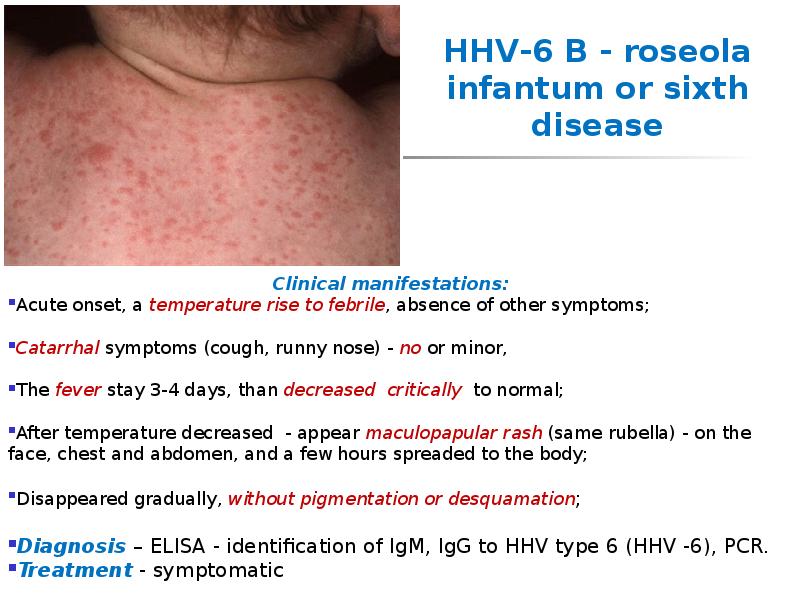
- 23. HHV-6 В - roseola infantum or sixth disease Clinical manifestations: Acute
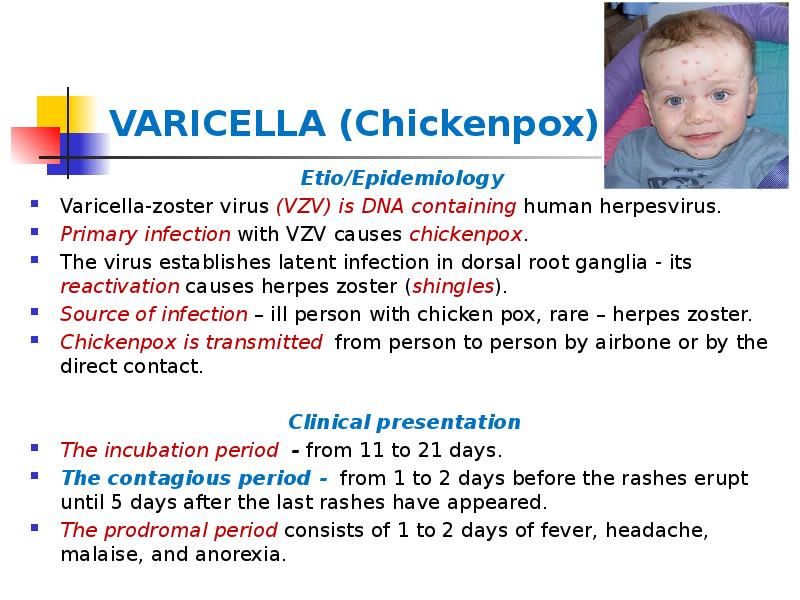
- 24. VARICELLA (Chickenpox) Etio/Epidemiology Varicella-zoster virus (VZV) is DNA containing human
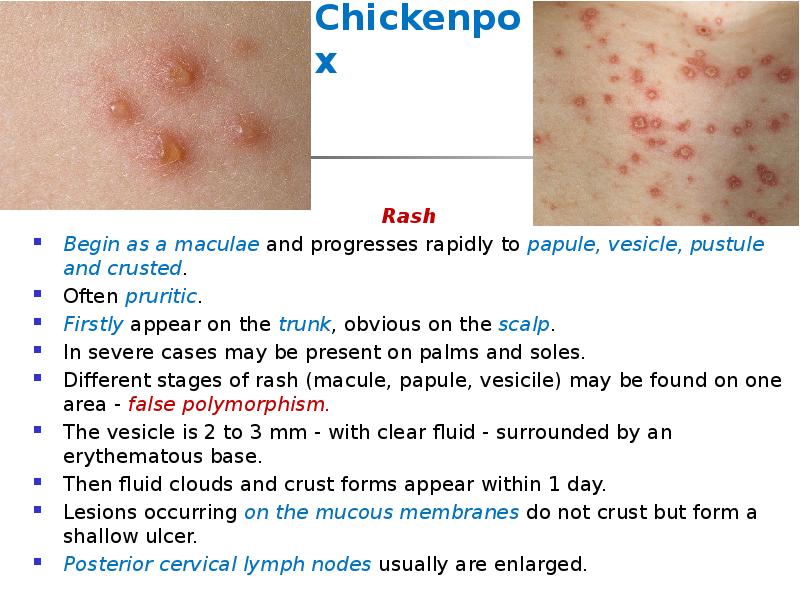
- 25. Chickenpox Rash Begin as a maculae and progresses rapidly to
- 26. Chickenpox
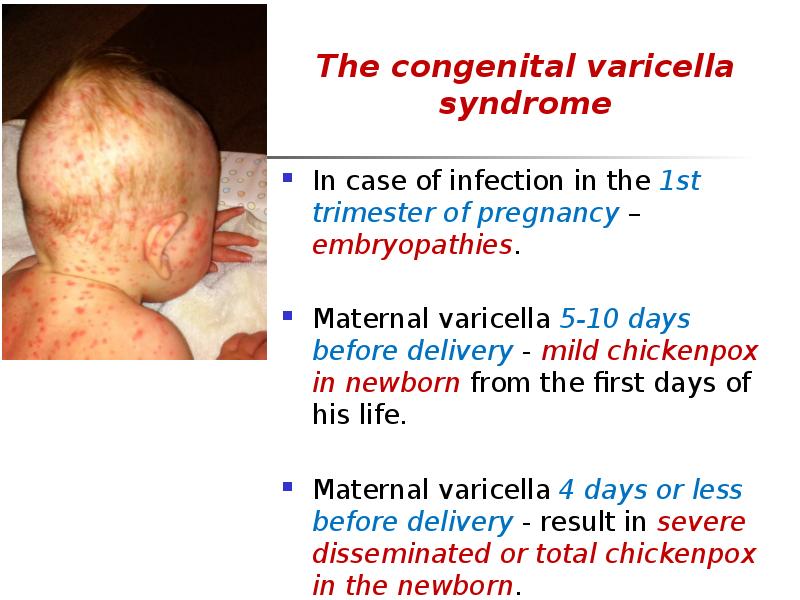
- 27. The congenital varicella syndrome The congenital varicella syndrome In case of
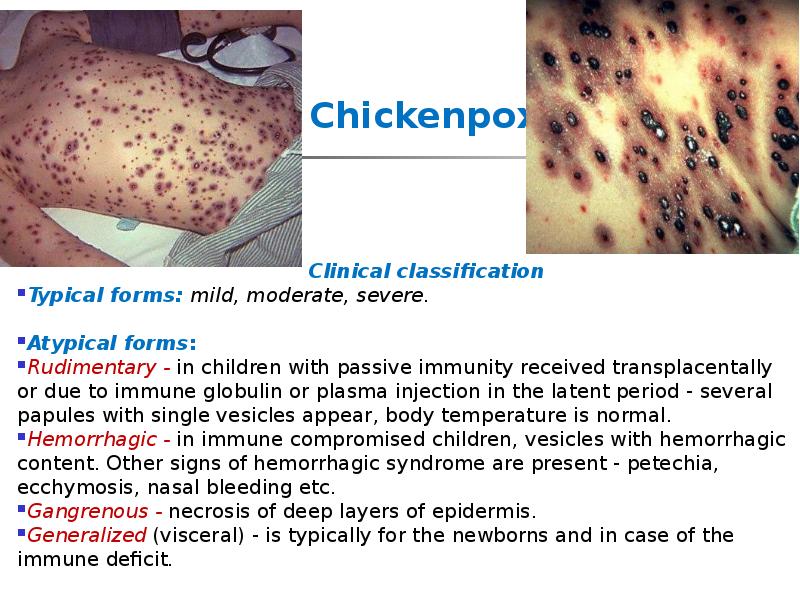
- 28. Chickenpox Clinical classification Typical forms: mild, moderate, severe.
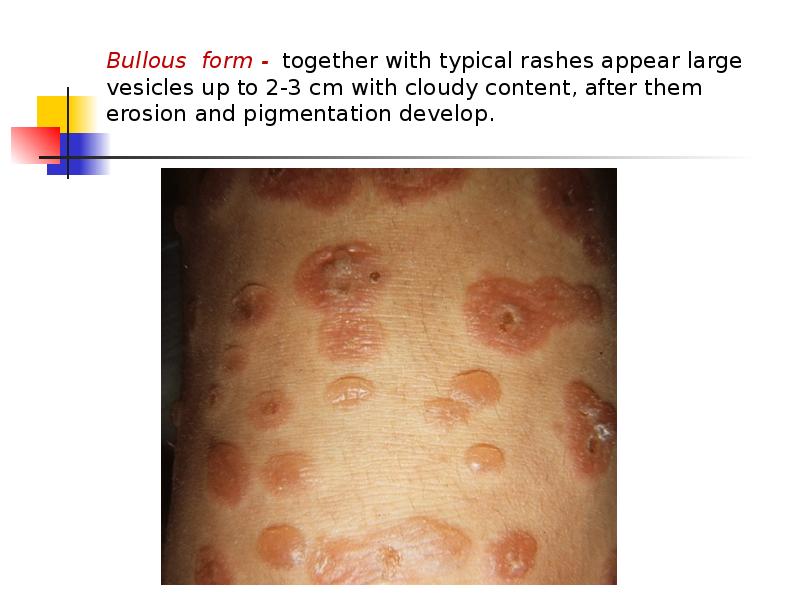
- 29. Bullous form - together with typical rashes appear large vesicles up
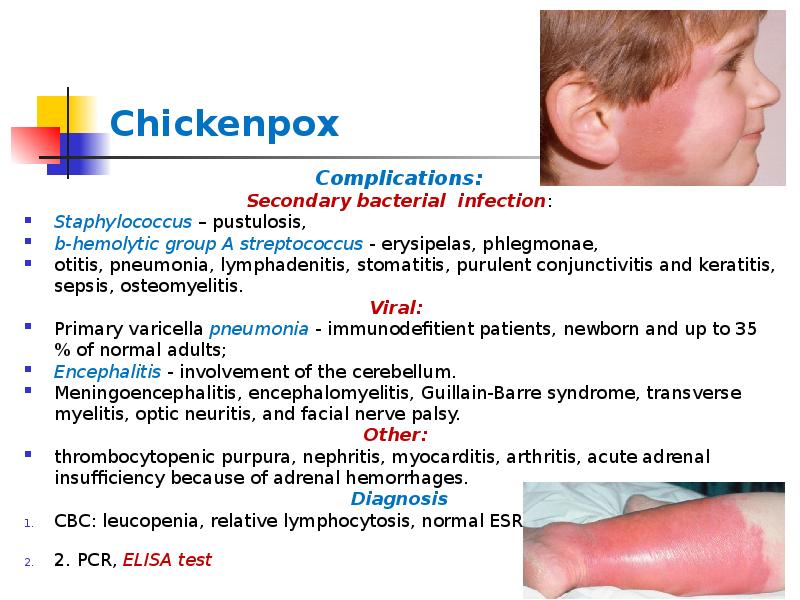
- 30. Chickenpox Complications: Secondary bacterial infection: Staphylococcus – pustulosis, b-hemolytic group A
- 31. Chickenpox Treatment Symptomatic up to disappear
- 32. Diagnosis? Simptom?
- 33. Sources
- 34. Скачать презентацию




Слайды и текст этой презентации
Похожие презентации