lecture kidney pathophysiology презентация
Содержание
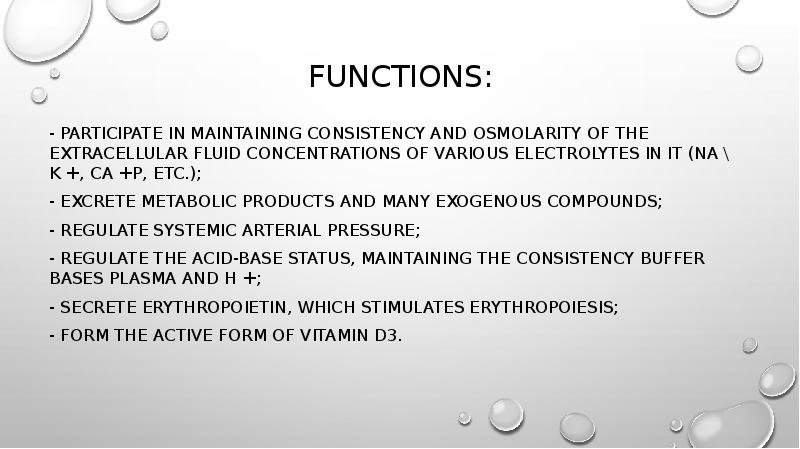
- 2. functions: - Participate in maintaining consistency and osmolarity of the
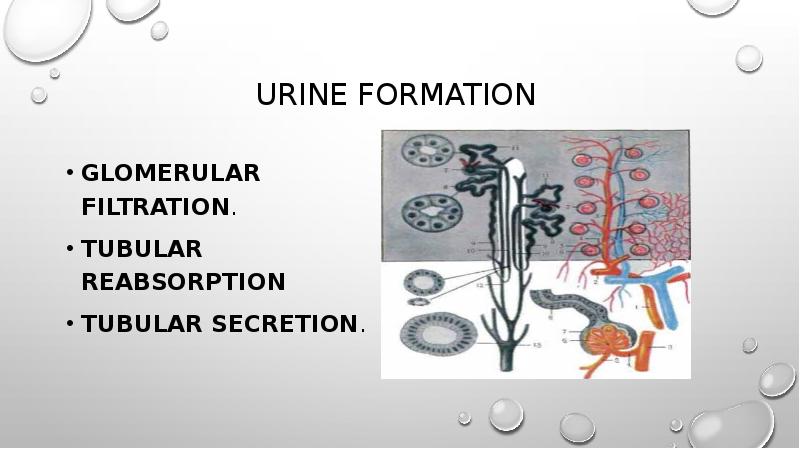
- 3. Urine formation Glomerular Filtration. Tubular Reabsorption Tubular Secretion.
- 4. Glomerular Filtration. As blood flows through the glomeruli, much of
- 5. Glomerular Filtration. The glomerulesfiltation can be decreased or increased. filtration
- 6. Glomerular Filtration. The increase in the volume of glomerular filtrate.
- 7. Tubular Reabsorption Is the movement of substances out of the renal
- 8. Tubular Secretion. Nephron tubule cells have the added capacity to extract
- 9. Changes in the composition of urine. Proteinuria. Normally, the penetration
- 10. Glomerular proteinuria is associated with increased permeability of the glomerular filter,
- 11. Hematuria (red blood cell) - a pathological phenomenon, characterized by
- 12. Diseases of the kidneys are divided into 2 major groups according
- 14. ACUTE NEPHRITIC SYNDROME. The nephritic syndrome is the result of
- 15. NEPHROTIC SYNDROME Nephrotic syndrome is a group of diseases having different
- 16. Odema results from salt and water retention and a loss of
- 17. The hyperlipidemia is characterized by elevated levels of triglycerides and
- 18. Hypercoaguability. At nephrotic syndrome may develop thrombosis as a result
- 19. tubulointerstitial pathology. Damage to tubulointerstitial tissues results in alterations in
- 21. ACUTE RENAL FAILURE Acute renal failure represents a rapid decline
- 22. The causes of acute renal failure Prerenal failure, the most common
- 23. 3 stages Oliguric stage: is characterized by urinary output of less
- 24. Chronic renal failure is a syndrome characterised by progressive and
- 25. 1.Decreased renal reserve. At this stage, damage to renal parenchyma is
- 27. Скачать презентацию







Слайды и текст этой презентации
Похожие презентации